2Department of Radiation Oncology, Urmia University of Medical Sciences, Urmia-İran DOI : 10.5505/tjo.2021.2709
Summary
OBJECTIVEAlthough technique improvements have drastically reduced radiotherapy (RT) related toxicity, most patients still experience burdensome RT side effects. Studies have shown an increase in distress, anxiety, fatigue, and depression in patients undergoing radiation. Radiation-induced side effects adversely affect quality of life for cancer survivors. This study aimed to determine the mood status in patients with gastrointestinal tract cancer undergoing RT.
METHODS
This randomized cross-sectional study conducted on 126 patients with gastrointestinal tract cancer undergoing
RT. We used a demographic form, and the Persian Version of Profile of Mood States 2nd edition
questionnaire for data collection.
RESULTS
The mean of total mood disturbance was 77.39±15.03. The results demonstrated there is a relationship
between tension-anxiety with; depression-dejection (DD), anger-hostility (AH), fatigue-inertia (FI); and
confusion-bewilderment (CB) (p<0.001). In addition, there was a significant relationship between DD
with AH, FI, and CB (p<0.001). There was also a significant relationship between AH with FI and CB
(p<0.001). In addition, there was a statistically significant relationship between FI with CB (p<0.001).
CONCLUSION
Our results suggested that there is a high prevalence of mood disturbance in patients with gastrointestinal
tract cancer undergoing RT. Therefore, applying strategies for improving mood are important
among these patients, because it can lead to better therapeutic outcomes.
Introduction
The results from Global Cancer Statistics 2018 showed that gastrointestinal cancers, including colorectal, stomach, and liver cancers, represent the most common causes of cancer death worldwide.[1] The risk of affliction with gastric cancer is higher in the northern and northwest of Iran, while it is moderate in the western and central provinces and low in the southern regions.[2]Radiotherapy (RT) is one of the treatment options that can be used alone or adjuvant in cancer. Combinations are varied, can be used before, during or after chemotherapy or surgery. In addition, it may be indicated for prophylaxis, reduction of tumor volume, total cure, or to avoid remission.[3] RT-induced fatigue (RIF) is a clinical subtype of cancer treatment-related fatigue. It is described as a pervasive, subjective sense of tiredness persisting over time, interferes with activities of daily living, and is not relieved by adequate rest or sleep. RIF is one of the early side effects and long-lasting for cancer patients treated with localized radiation.[4] RIF is a serious clinical problem, and its cause is multifactorial, in which several mechanisms have been proposed, including genetic, inflammatory, immunological, psychological, hormonal factors, and hemoglobin levels. All of these etiological factors in fatigue related to RT play relevant roles in impairment of oxygen delivery, weight and appetite loss and neuromuscular fatigue. As well as, low levels of physical activity, mass and muscle strength can cooperate for fatigue.[3] Fatigue is the most common symptom experienced by patients during the cancer trajectory from diagnosis to the end of life.[5] Hence, fatigue is an important symptom in caring of patients with cancer.[6] In addition, regardless of treatment site, RT has been reported to cause acute fatigue in up to 80% of patients, and chronic fatigue can persist in up to 30% for months to years after treatment.[7] Furthermore, fatigue can a?ect the feelings, daily activities, social relationships, and treatment period.[8]
On the other hand, anxiety and depression are disabling, underdiagnosed issues that affect the management of oncology patients.[9] Oncologic patients undergoing radiation therapy are at high risk for mental health disorders such as distress, anxiety, and depression.[7,9-11] Evidence shows that early treatment and diagnosis of anxiety and depression reduce clinical morbidity and improves patient outcomes.[9] Although such problems tend to decrease upon RT completion, a significant number of patients still manifest psychological effects after treatment. Patients with pancreatic cancer appear particularly vulnerable, higher rates of depression being associated with those diagnoses.[7] Hence, this randomized cross-sectional study aimed to determine the mood status in patients with gastrointestinal tract cancer undergoing RT. Our research question was: How is the mood status in patients with gastrointestinal tract cancer undergoing RT?
Methods
Ethical ConsiderationsThis study obtained the approval from the Research Ethics Committee of affiliated University (the ethics approval reference number of this study is IR.UMSU. REC 1399, 004). Patients received written information and were allowed 3 days to consider their decision. All patients were instructed that they could withdraw from the research at any time. All participants provided their written, informed consent to take part in this research.
Design of Study and Participants
Eligible patients (based on inclusion criteria) who
started their RT between October 2018 and June 2020
were selected randomly for this randomized cross-sectional
study.
The inclusion criteria were signed and dated informed consent form before study entry; histologically or cytologically confirmed one of the gastrointestinal tract cancers (esophageal cancer, gastric [stomach] cancer, colorectal cancer, pancreatic cancer, liver cancer in Stages I, II, or III), age between 35 and 70 years (the age range of GI cancer was between 40 and 70 years in our city just before this study, so we decided to selecting this age range for increasing chance of sampling), actively undergoing radiation therapy at the time of the study, and having history of RT (at least one session).
The exclusion criteria were serious comorbidities; concurrent chemo-RT, concomitant neurologic conditions that would complicate interpretation; other active malignancies; treatment with antiepileptic drugs, antidepressants, and major analgesics (unless stable dosing and conditions have been reached); active infection; severe lung disease; uncontrolled hypertension or diabetes; bleeding disorders requiring blood transfusion; and patients who had major surgery within 4 weeks, or thromboembolic events of Grade 3 or higher within 6 months before study entry.
Sample Size
Considering the study of Bueno-Robles and Soto-
Lesmes[12] entitled "Mood State of Women with Breast
Cancer and that of Their Spouses," the minimum sample
size for achieving power of 80% for a confidence
interval of 95% based on the following formula calculated;
125 patients for our study.
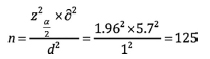
And a total of 126 patients with gastrointestinal cancer were recruited in this study.
Data Collection and Measurements
We used a demographic form, and Profile of Mood States
2nd edition (POMS2) questionnaire for data collection.
The POMS2 instruments assess the mood states of individuals 13 years of age and older. The POMS2 designed to evaluate individuals within six different mood domains: Anger-hostility (AH), confusion-bewilderment (CB), depression-dejection (DD), fatigueinertia (FI) tension-anxiety (TA), and vigor-activity (VA). The scale has been recommended for evaluating affective changes over the course of brief treatment or assessment period.
The instruments are a collection of self-rating tools that allow for the quick assessment of transient, fluctuating feelings, and enduring affect states. The tool is applicable in clinical, medical, research, and athletic settings, where its sensitivity to change makes the assessment ideal for treatment monitoring and evaluation, as well as clinical trials.
Scores on these items are added together to determine a Total Mood Disturbance score. The POMS2 is an adjective checklist with instructions to respond "How have you been feeling over the PAST WEEK, INCLUDING TODAY" on a 5-point Likert response scale ranging from 0=Not at all, to 4=Extremely.
Hence, the range of calculated total mood disturbance score based on POMS2 questionnaire is between -32 and 200. The tool is available in an online, as well as a pen-and-paper format.[13,14]
We used the Persian Version of POMS2, has been used by Khoshnoudfar et al.[15] in 2019 and its reliability that was evaluated using Cronbach"s alpha method (by Khoshnoudfar et al.) was 0.91.
The Study Procedure
In this study, patients completed a demographic questionnaire
first, which included questions pertaining to
the patient"s age, sex, education level, marital status,
employment status, duration of disease after diagnosis,
and other information. Then a researcher administered
the POMS 2 questionnaire at the RT centers. The item
s of questionnaires read to patients with low levels of
education, and their verbal responses were recorded.
Statistical Analysis
Descriptive statistics such as frequency distribution tables
and central and dispersion indices were used for
categorization and summarization of data. To examine the quantitative and qualitative variables of the study,
first the normality of these variables was examined by
Kolmogorov-Smirnov test. Independent t-test, analysis
of variance (ANOVA), and Pearson correlation coefficient
used to test the research hypotheses. Significance
level was considered for all tests with p<0.05.
Results
Demographic Variables and Clinical Characteristics of the ParticipantsIn the present study, 54.8% of the participants were male, 84.3% of the participants were married, and 10% had university diploma. In addition, 59.2% of the participants were unemployed. In addition 67.1% of patients were in Stage I of cancer. The mean of body mass index was 22.31±3.84. The mean of age was 55.72±5.51 years in the male participants and it was 54.03±6.94 years in female participants.
In addition, 36% of the participants had gastric cancer, 32% had esophageal cancer, 24% had rectum cancer, and 8% had colon cancer.
In terms of sex, the subjects were divided into two groups of males and females. Mean mood scores in the two groups were assessed using independent t-test. The results of t-test showed that there was no significant difference in mood scores between males and females (p=0.625). Independent t-test showed that mood scores between the two groups of marital status (single and married people) were not significantly different from each other (p=0.347). Examination of research units in terms of education level using ANOVA showed that mood scores at different levels of education did not differ significantly (p=0.733). The employment status of research units was examined at both employed and non-employed levels. The results of independent ttest showed that mood scores between employed and non-employed individuals were not significantly different from each other (p=0.512). The study units were grouped into urban and rural groups in terms of housing status. The results of independent t-test showed that mood scores were not significantly different between urban and rural people (p=0.175). We used t-test to examine the difference in mood scores between people who had health insurance and people who did not have health insurance. The results showed that the mood scores between these two groups were statistically the same and did not differ significantly (p=0.291). The research units were examined at different levels of income level. The results of independent t-test showed that there was no significant difference between the mood scores in the two levels of income less than expenses and income more than expenses (p=0.078). ANOVA was used to evaluate the difference between the mean mood score in different stages of cancer. The results showed that the mood score in the three levels stages of cancer was not significantly different from each other (p=0.426). The mean mood score was not significantly different between people with a history of similar illness in the family and people without a history (p=0.750) (Table 1).
Table 1: Frequency distribution of mood score among the studied variables
Profile of Mood Statesbr> As it shown in Table 2; the mean of Total Mood Disturbance was 77.39±15.03, with the minimum of 22, and the maximum of 137. The mean of TA was 16.76±3.56. The mean of DD was 26.46±5.39. The mean of AH was 21.33±4.33. The mean of FI was 12.90±3.34. The mean of CB was 12.73±2.80, and the mean of VA was 12.49±3.81 (Table 2).
Table 2: Frequency distribution of mood domains
As it shown in Table 3; we used Pearson correlation coefficient to examine the relationship between mood domains. The results demonstrated there is a relationship between TA with; DD, AH, FI and CB (p<0.001). In addition, there was a significant relationship between DD with AH, FI and CB (p<0.001). There was also a significant relationship between AH with FI and CB (p<0.001). Furthermore, there was a statistically significant relationship between FI with CB (p<0.001) (Table 3).
Table 3: The relationship between different mood domains
Furthermore, based on regression test results for predicting of mood scores based on domains in patients with gastrointestinal tract cancers (Table 4) it was concluded that six domains of mood (CB, DD, TA, FI, AH, and VA) can predict 97% of mood score"s variance. Furthermore, regarding beta and P values, all of mood domains, excluding CB were statistically significant (Table 4).
Discussion
In our study that was conducted in the northwest of Iran 36% of the participants had gastric cancer, 32% had esophageal cancer, 24% had rectum cancer, and 8% had colon cancer. But in the study of Hedayatizadeh- Omran et al.[2] in the north of Iran the most prevalent cancers included gastric cancer (44.2%), colorectal cancer (27.2%), and esophageal cancer (13.5%).Oncology patients frequently experience psychological as well as somatic distress. However, they feel that their emotional needs are most frequently neglected in the medical care programs they undertake. [16] Hence, this randomized cross-sectional study aimed to determine the mood status in patients with gastrointestinal tract cancer undergoing RT.
Our results is consistent with the study of Ghasemi and Hatamian that demonstrated; there was a significant relationship between psychological symptoms, including depression, stress, and anxiety with fatigue in gastrointestinal cancer patients (p<0.05). They concluded; the severity of fatigue is related to the extent of psychological symptoms (depression, anxiety, and stress) in patients with cancer. A patient's depression and anxiety predicts the fatigue.[17] In addition, our research is similar to the study of Ünsal et al.[18] that demonstrated: The fatigue rate increases during RT in patients with cancer.
Cancer is a life-threatening and feared diagnosis and is a source of great distress in patients. A cancer diagnosis generates a higher sense of distress than non-neoplastic diseases with poorer prognoses. [19] Several studies have demonstrated that 30-40% of patients with cancer report emotional distress as a consequence of the disease and treatment, many of whom meet the criteria for adjustment, anxiety, and depressive disorders.[20,21] Psychological distress, a common yet treatable condition in individuals with cancer, is associated with suffering and poor outcomes.[22] Depression is a common psychiatric manifestation occurring during and also after cessation of cancer therapy,[23,24] accordingly the results of our study demonstrated there is a relationship between TA with; DD, AH, FI, and CB. In addition, there was a significant relationship between DD with AH, FI, and CB. There was also a significant relationship between AH with FI and CB. There was also a statistically significant relationship between FI with CB.
In addition a randomized controlled trial conducted by Guo et al.[25] on cancer patients undergoing RT, demonstrated that a psychosocial intervention significantly reduced levels of depression and anxiety. Furthermore, the intervention was effective for improving elements of quality of life, such as global health status and physical functioning; it also increased emotional functioning, significantly decreased insomnia both during and after RT, and was similar in cost-effectiveness.
Limitations
The generalizability of our findings may be limited.
One of limitations is relatively small sample size.
Another limitation is using self-reporting POMS2
questionnaire, without applying other tools for evaluation
of RIF. Hence, it is suggested; other study with
bigger sample size, using electrophysiological methods
for evaluation of fatigue conducted.
Conclusion
This randomized cross-sectional study demonstrated; RT has a strong negative impact on the mood domains of patients with gastrointestinal tract cancer, which can lead to decreased quality of life and refusing treatment.Due to increasing number of these patients, improving health and reducing RT complications are important issues. Comparing the results of the present study with previous studies, it seems that prolonging the course of treatment due to RT side effects causes mood disturbance in patients that can affect other aspects of their lives. Therefore, applying strategies for improving mood are important in patients with gastrointestinal tract cancer undergoing RT, because these strategies can lead to better therapeutic outcomes.
Peer-review: Externally peer-reviewed.
Conflict of Interest: All authors declared no conflict of interest.
Ethics Committee Approval: The study was approved by the Urmia University of Medical Sciences Research Ethics Committee (No: IR.UMSU.REC 1399, 004, Date: 17/03/2020).
Financial Support: None declared.
Authorship contributions: Concept - H.G., M.R.; Design - H.G., T.T., M.R.; Supervision - H.G.; Funding - None; Materials - M.M., T.T., M.R.; Data collection and/or processing - T.T., H.R.K.; Data analysis and/or interpretation - T.T., H.R.K.; Literature search - T.T., H.G.; Writing - T.T., H.G.; Critical review - T.T., H.G., M.R., M.M., H.R.K.
References
1) Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA,
Jemal A. Global cancer statistics 2018: GLOBOCAN
estimates of incidence and mortality worldwide
for 36 cancers in 185 countries. CA Cancer J Clin
2018;68(6):394-424.
2) Hedayatizadeh-Omran A, Yaghoubi-Ashrafi M, Qazizadeh
Z, Mousavi RS, Shekarriz R, Eslami M, et al.
Epidemiology of gastrointestinal cancers in the North
of Iran: Results of mazandaran population-based cancer
registry. Turk J Oncol 2020;35(4):414-21.
3) Passos CS, Sady ER, Neves RV, Carvalho BE, Costa
TS, Haro AS, et al. Cancer and radiotherapy-related
fatigue: Implications and therapies integratives. J Med
Oncl Ther 2018;3(1):9-14.
4) Hsiaoa CP, Dalya B, Saliganb LN. The etiology and
management of radiotherapy-induced fatigue. Expert
Rev Qual Life Cancer Care 2016;1(4):323-8.
5) Fabi A, Bhargava R, Fatigoni S, Guglielmo M, Horneber
M, Roila F, et al. Cancer-related fatigue: ESMO clinical
practice guidelines for diagnosis and treatment. Ann
Oncol 2020;31(6):713-23.
6) Kudubeş AA. Cancer-related fatigue of child and nursing
care. Turk J Oncol 2014;29(3):120-4.
7) Dilalla V, Chaput G, Williams T, Sultanem K. Radiotherapy
side effects: Integrating a survivorship
clinical lens to better serve patients. Curr Oncol
2020;27(2):107-22.
8) Yorulmaz H. Evaluation of factors affecting fatigue
and anxiety in patients with cancer. Turk J Oncol
2019;34(3):145-52.
9) Holtzman AL, Pereira DB, Yeung AR. Implementation
of depression and anxiety screening in patients
undergoing radiotherapy. BMJ Open Qual
2018;7(2):e000034.
10) Takahashi T, Hondo M, Nishimura K, Kitani A, Yamano
T, Yanagita H, et al. Evaluation of quality of life
and psychological response in cancer patients treated
with radiotherapy. Radiat Med 2008;26(7):396-401.
11) Stiegelis HE, Ranchor AV, Sanderman R. Psychological
functioning in cancer patients treated with radiotherapy.
Patient Educ Couns 2004;52(2):131-41.
12) Bueno-Robles LS, Soto-Lesmes VI. Mood state of
women with breast cancer and that of their spouses.
Invest Educ Enferm 2016;34(3):537-43.
13) Shahid A, Wilkinson K, Marcu S, Shapiro CM. Profile
of mood states (POMS). In: Shahid A, Wilkinson
K, Marcu S, Shapiro C, editors. STOP, THAT and One
Hundred Other Sleep Scales. New York: Springer;
2011.
14) Lin S, Hsiao YY, Wang M. Test review: The profile
of mood states 2nd Edition. J Psychoeduc Assess
2014;32(3):273-7.
15) Khoshnoudfar Z, Omidvar B, Tahmasebi S. The relationship
between self-compassion and spiritual health
with quality of life and mood in women with breast
cancer. Sadra Med J 2019;7(1):23-36.
16) Mannarini S, Polimeni S, Shams M, Giacobbo M.
Assessing negative and positive mood states: The identification
of a short form of the POMS scale in Italian
oncology outpatients. TPM 2012;19(2):135-45.
17) Ghasemi A, Hatamian H. The relationship between
fatigue and psychological symptoms in patients
with gastrointestinal cancer. Caspian J Neurol Sci
2016;2(5):29-35.
18) Ünsal D, Aksu A, Bagriacik U, Akmansu M. The fatigue
rate and association with serum cytokine and
leptin levels in breast cancer patients undergoing postmastectomy
radiotherapy: A prospective evaluation.
Turk J Onkol 2007;22(1):1-12.
19) Smith HR. Depression in cancer patients: Pathogenesis,
implications and treatment (Review). Oncol Lett
2015;9(4):1509-14.
20) Chaitanya NC, Garlapati K, Priyanka DR, Soma S,
Suskandla U, Boinepally NH. Assessment of anxiety
and depression in oral mucositis patients undergoing
cancer chemoradiotherapy: A randomized cross-sectional
study. Indian J Palliat Care 2016;22(4):446-54.
21) Grassi L, Johansen C, Annunziata MA, Capovilla E,
Costantini A, Gritti P, et al. Screening for distress in
cancer patients: A multicenter, nationwide study in
Italy. Cancer 2013;119(9):1714-21.
22) Pirl WF, Fann JR, Greer JA, Braun I, Deshields T,
Fulcher C, et al. Recommendations for the implementation
of distress screening programs in cancer
centers: Report from the American psychosocial oncology
society (APOS), Association of oncology social
work (AOSW), and oncology nursing society (ONS)
joint task force. Cancer 2014;120(19):2946-54.
23) Chen SC, Lai YH, Liao CT, Lin CC, Chang JT. Changes
of symptoms and depression in oral cavity cancer
patients receiving radiation therapy. Oral Oncol
2010;46(7):509-13.





